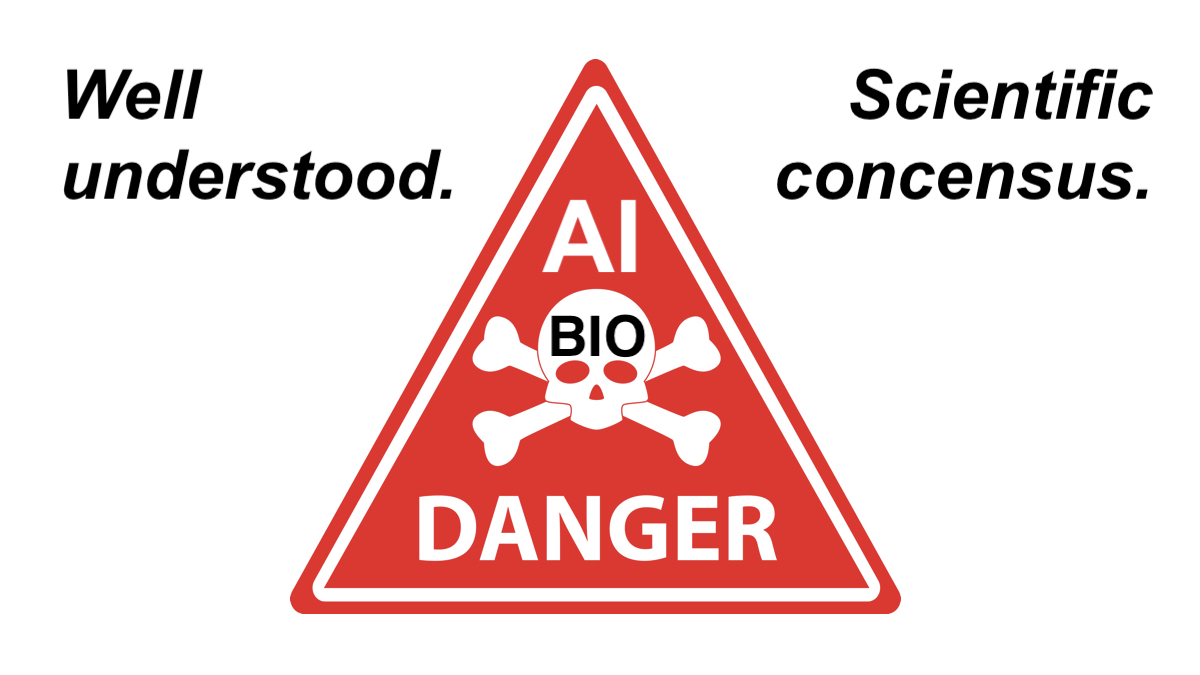
WARNING. EXISTENTIAL RISK. Natural or Man-made… the NEXT PANDEMIC is CERTAINLY Coming.
THE MAN-MADE RISK: Currently unregulated easily available and uncontained AI Technology combined with powerful advances in Biotechnology create an existential threat to billions of people from potential bio-terrorist actors’ creation of synthetic pathogens, poisons and other unpredictable bio-weapons of mass death and disruption.
COVID-19 COST more than $25 TRILLION and 25 MILLION DEATHS with a case-fatality-rate of about 0.5%
The case-fatality-rate of BIRD FLU is about 60%.
Learn more:
The Containment Problem and The Coming Wave by Mustafa Suleyman
By KATE BINGHAM and TIM HAMES
PUBLISHED: 23:07, 22 September 2023
Adapted from The Long Shot: The Inside Story of the Race to Vaccinate Britain by Kate Bingham & Tim Hames (Oneworld Publications, £10.99). © Kate Bingham & Tim Hames 2023.
The next major pandemic is coming. It’s already on the horizon, and could be far worse — killing millions more people — than the last one.
We don’t yet know for certain what form it will take — just that its arrival, according to global health experts, is not just a possibility but a probability.
That’s horrific enough. Even more terrifying is the fact that Britain and the rest of the world have so far done very little to prepare for it.
To combat Disease X — as the World Health Organisation ominously calls it — we will once again need vaccines to be engineered and delivered in record time. But, as things stand, there is absolutely no guarantee that will happen.
By contrast, we may well look back at the Covid-19 crisis as a walk in the park — and of course it was nothing of the kind.
Today, it’s all too easy to forget that governments around the world were dangerously unprepared for a global health crisis; indeed many viewed it as the stuff of apocalyptic fiction.
Let me remind you of the state we were in by May 2020. The outlook was unremittingly bleak: infections and deaths were mounting inexorably and hospitals were at breaking-point. The pandemic had ruptured economic activity more than any recession.
Mass vaccination was the only credible solution, but no human coronavirus vaccine had ever been approved, let alone one for Covid-19. Worse, the historic success rate for any new vaccines, from lab to jab, was a deeply depressing 10 per cent. So the scale of the challenge was stupendous.
It was in May that the then Health Secretary Matt Hancock phoned me out of the blue, asking me to become head of the new Vaccine Taskforce. I immediately took leave of absence from my job of nearly 30 years as a biotech venture capitalist — dealing with the development of new drugs — to work on finding a portfolio of vaccines, in the hope that at least one would be effective.
While scientists around the world threw themselves into developing possible vaccines at what seemed like warp speed, the taskforce worked around the clock to prioritise the best candidates at early stages, to check they were both safe and effective, to make binding deals in the face of international competition and to ensure the vaccines could be manufactured at scale.We all know what happened a few months later: two of the taskforce’s chosen vaccines were approved by regulators. And, in December 2020, the UK became the first country in the world to launch its vaccination programme.
Believe me, none of that was inevitable. Nor should we be complacent now that Covid-19 is largely regarded as a routine illness, even though it can still kill the vulnerable and elderly.
Scientists know that it could still mutate into new variants that are more infectious and even better at evading our immune systems. What this means is that we could soon face new viral mutants resistant to all the antiviral drugs and vaccines we’ve managed to develop so far.
But even mutated variants of Covid-19 pale in comparison to the other viral threats out there.
Let me put it this way: the 1918–19 flu pandemic killed at least 50 million people worldwide, twice as many as were killed in World War I. Today, we could expect a similar death toll from one of the many viruses that already exist.
The whole point of a virus is to replicate as many times as possible in as many hosts as possible. So they are continually mutating and latching on to different animals.
In fact, some of the most dangerous viruses — such as smallpox, measles, Ebola and HIV — originated in animals and later became highly transmissible between humans.
Today, there are more viruses busily replicating and mutating than all the other life forms on our planet combined. Not all of them pose a threat to humans, of course — but plenty do.
So far, scientists are aware of 25 virus families, each of them comprising hundreds or thousands of different viruses, any of which could evolve to cause a pandemic.
Worse still, they estimate there could be more than one million undiscovered viruses which may be able to jump from one species to another, mutate dramatically and kill millions of human beings.
Why were we so surprised when Covid-19 struck in 2020? It wasn’t as if we were being attacked out of the blue — say, by a giant asteroid or aliens from another planet.
In fact, the warning shots had already been fired. We knew that Covid — or something like it — was likely to arrive sooner rather than later because the pace of pandemics had been quickening over the past few decades.
Unlike an epidemic, which is contained in a single country or region, a pandemic spreads across many countries and even continents. Covid-19 was actually the seventh outbreak of a pandemic since the millenium.
It had been preceded by SARS in 2002–4, H5N1 bird flu in 2004, H1N1 swine flu in 2009, MERS in 2012, Ebola in 2014–16 and Zika in 2015–16.
What stopped these outbreaks wreaking global havoc was usually one or more of these factors: poor infectivity (MERS), a relatively low fatality rate (swine flu) or a swift, co-ordinated international response (SARS). In other words, good luck and good preparation working in tandem.
In a sense, we got lucky with Covid-19, despite the fact that it caused 20 million or more deaths across the world. The point is that the vast majority of people infected with the virus managed to recover.
Ebola, on the other hand, has a fatality rate of around 67 per cent. Bird flu is not far behind at 60 per cent. Even MERS hit 34 per cent.
So we certainly can’t bank on the next pandemic being easily contained.
Imagine Disease X is as infectious as measles with the fatality rate of Ebola. Somewhere in the world, it’s replicating, and sooner or later, somebody will start feeling sick.
So why are pandemics on the increase? Well, I can assure you that we’re not simply experiencing a random patch of bad luck.
The increase in outbreaks is the price we’re having to pay for living in the modern world. First, it’s increasingly connected through globalisation. Second, more and more people are cramming into cities, where they often come into close contact with others.
And third, millions of acres of natural habitat are being destroyed by us each year. This reason is particularly important, because around three-quarters of emerging infectious diseases originate in animals and then leap from species to species until they can, in certain circumstances, infect human beings.
Through deforestation, modern agricultural methods and the destruction of wetlands, we are creating the ideal conditions for these species jumps to take place.
Why? Because massive loss of habitat is pushing animals into ever closer proximity to different species — including us. It’s a virus’s idea of paradise.So what’s to be done? Crucially, we need to take the first steps in dealing with the next pandemic right now — and that involves putting money on the table.
Pandemic viruses have a lot in common with software viruses, which most of us take very seriously. So we invest in the appropriate software, and we update it regularly on our phones, tablets, laptops and desktops.
We don’t just sit back and hope we’ll never be victims of a computer virus attack. On the contrary, most of us spend quite a bit to ensure we won’t.
In 2020, the cybersecurity market globally was valued at a little under $170 billion; at current growth rates it will hit almost $370 billion by 2028. That’s an astonishing amount of money.
Yet there’s very little evidence that we’re prepared to spend anything remotely comparable on protecting ourselves from real viruses — the ones that could kill us.
Yet the monetary cost of inaction is seismic. After all, even Covid-19 — a milder virus than Disease X — managed to leave us holding a bill for $16 trillion in both lost output and public health expenditure.
That’s why we need to discover — in advance of the next pandemic — a collection of different prototype vaccines for every threatening virus family that we know about. We’d then have a head start — because we’d be able to engineer those vaccines to target the very specific features of Disease X.
Impossible? Not at all.
The reason why there was such a rapid global response to Covid-19 was because frameworks had already been developed a decade earlier as part of the (unsuccessful) process to develop vaccines against SARS and MERS.
So when Covid-19 emerged, scientists already had a prototype design that could be modified to deal with the new virus.
Developing appropriate vaccines in less than a year was something of a miracle. Yet even that speed would be insufficient if the next pandemic turns out to be far more lethal than the last.
When I led the Vaccine Taskforce, a central feature of our approach was to build a portfolio of different types of vaccines. In 2020, we didn’t know which, if any, format of vaccine was going to work against Covid-19 and its variants, so we wanted to deploy a breadth of different approaches.
To deal with Disease X, we’ll again need a portfolio strategy.
First, because different types of vaccines stimulate different immune responses and therefore they provide different levels of protection.
Second, manufacturing capabilities vary enormously across countries and regions.
Some vaccine formats may be suitable for large-scale production, while others may be easier to produce in the third world.
We saw this with Covid-19, where it made sense to use Pfizer-BioNTech and Moderna in wealthier nations and Oxford-AstraZeneca in poorer places.
Third, we need to address the shortcomings of current vaccines, not all of which are durable, easy to transport or cheap.
Fourth, researchers must be encouraged to trial new technologies and approaches to vaccine design, potentially leading to more effective and efficient vaccines in the future.
Vaccines aren’t the only answer, of course. We urgently need to invest in state-of-the-art systems for international surveillance of prospective virus threats.
Ideally, Disease X will be neutralised before it starts spreading across the globe and mutating (which it certainly will, if left unchecked).
We also need to think again about what can be done during the period after Disease X hits Britain, and before an effective vaccine can be rolled out.
In 2020, we had no experience of lockdowns, so it was painfully obvious that policy was made up on the hoof. No such excuse next time.
Before it even enters Britain, we need to have rehearsed our response much better and more scientifically. Was it right to close schools? To lock down for long periods? To ban travel? Advise people to wear masks?
Researchers are working on these questions, among others. But there should be no restrictions on who can work on the data from the last pandemic — it should be made available in a central database to scientists around the world.
We need to go even further. One of the many tragedies of the 2020 Covid-19 saga was that countries often retreated into silos and failed to support any serious international plan. It was a major failure, which cost many lives.
To provide vaccines at low cost, we must build biological vaccine-manufacturing capacities in countries from each continent, and organise robust training. Ideally, the countries selected would be ones with low populations.
Why? Because there would be less chance of political demands to ‘vaccinate our own people first’ rather than treating those most in need. The vaccine nationalism of 2020, one hopes, would become a thing of the past.
This really is no time for complacency. We’ve already experienced a relatively non-lethal pandemic, and governments are aware that the next one could be far worse.
The logical next step is to have a single global body responsible for our response to Disease X. The obvious one to take up the mantle is the Coalition for Epidemic Preparedness Innovations (CEPI), working in close conjunction with the World Health Organisation.
Truly international, CEPI was launched at Davos in 2017 to develop vaccines against future epidemics. It is currently working on a five-year plan to compress vaccine development to 100 days and create a library of vaccines.
We will also need to fund a global budget for this body, with contributions based on national wealth.
Finally, all of them should agree to sign up to a Global Pandemic Treaty. This would enable the open sharing of information among scientists and clinicians, and give clear accountability for vaccine development and manufacturing.
A tall order? Perhaps — but not an impossible one.
The remarkable success of the scientific drive against Covid-19 shows what can be achieved when we pull together. But next time, we need to be far better and far faster.
Learn more:
The Containment Problem and The Coming Wave by Mustafa Suleyman
By KATE BINGHAM and TIM HAMES
PUBLISHED: 23:07, 22 September 2023 | UPDATED: 02:57, 23 September 2023
Adapted from The Long Shot by Kate Bingham & Tim Hames (Oneworld Publications, £10.99). © Kate Bingham & Tim Hames 2023. To order a copy for £9.89 (offer valid to 07/10/2023; UK P&P free on orders over £25) go to mailshop.co.uk/books or call 020 3176 2937.
The Long Shot: The Inside Story of the Race to Vaccinate Britain
The next major pandemic is coming. It’s already on the horizon, and could be far worse — killing millions more people — than the last one.
We don’t yet know for certain what form it will take — just that its arrival, according to global health experts, is not just a possibility but a probability.
That’s horrific enough. Even more terrifying is the fact that Britain and the rest of the world have so far done very little to prepare for it.
To combat Disease X — as the World Health Organisation ominously calls it — we will once again need vaccines to be engineered and delivered in record time. But, as things stand, there is absolutely no guarantee that will happen.
By contrast, we may well look back at the Covid-19 crisis as a walk in the park — and of course it was nothing of the kind.
Today, it’s all too easy to forget that governments around the world were dangerously unprepared for a global health crisis; indeed many viewed it as the stuff of apocalyptic fiction.
Let me remind you of the state we were in by May 2020. The outlook was unremittingly bleak: infections and deaths were mounting inexorably and hospitals were at breaking-point. The pandemic had ruptured economic activity more than any recession.
Mass vaccination was the only credible solution, but no human coronavirus vaccine had ever been approved, let alone one for Covid-19. Worse, the historic success rate for any new vaccines, from lab to jab, was a deeply depressing 10 per cent. So the scale of the challenge was stupendous.
It was in May that the then Health Secretary Matt Hancock phoned me out of the blue, asking me to become head of the new Vaccine Taskforce. I immediately took leave of absence from my job of nearly 30 years as a biotech venture capitalist — dealing with the development of new drugs — to work on finding a portfolio of vaccines, in the hope that at least one would be effective.
While scientists around the world threw themselves into developing possible vaccines at what seemed like warp speed, the taskforce worked around the clock to prioritise the best candidates at early stages, to check they were both safe and effective, to make binding deals in the face of international competition and to ensure the vaccines could be manufactured at scale.We all know what happened a few months later: two of the taskforce’s chosen vaccines were approved by regulators. And, in December 2020, the UK became the first country in the world to launch its vaccination programme.
Believe me, none of that was inevitable. Nor should we be complacent now that Covid-19 is largely regarded as a routine illness, even though it can still kill the vulnerable and elderly.
Scientists know that it could still mutate into new variants that are more infectious and even better at evading our immune systems. What this means is that we could soon face new viral mutants resistant to all the antiviral drugs and vaccines we’ve managed to develop so far.
But even mutated variants of Covid-19 pale in comparison to the other viral threats out there.
Let me put it this way: the 1918–19 flu pandemic killed at least 50 million people worldwide, twice as many as were killed in World War I. Today, we could expect a similar death toll from one of the many viruses that already exist.
The whole point of a virus is to replicate as many times as possible in as many hosts as possible. So they are continually mutating and latching on to different animals.
In fact, some of the most dangerous viruses — such as smallpox, measles, Ebola and HIV — originated in animals and later became highly transmissible between humans.
Today, there are more viruses busily replicating and mutating than all the other life forms on our planet combined. Not all of them pose a threat to humans, of course — but plenty do.
So far, scientists are aware of 25 virus families, each of them comprising hundreds or thousands of different viruses, any of which could evolve to cause a pandemic.
Worse still, they estimate there could be more than one million undiscovered viruses which may be able to jump from one species to another, mutate dramatically and kill millions of human beings.
Why were we so surprised when Covid-19 struck in 2020? It wasn’t as if we were being attacked out of the blue — say, by a giant asteroid or aliens from another planet.
In fact, the warning shots had already been fired. We knew that Covid — or something like it — was likely to arrive sooner rather than later because the pace of pandemics had been quickening over the past few decades.
Unlike an epidemic, which is contained in a single country or region, a pandemic spreads across many countries and even continents. Covid-19 was actually the seventh outbreak of a pandemic since the millenium.
It had been preceded by SARS in 2002–4, H5N1 bird flu in 2004, H1N1 swine flu in 2009, MERS in 2012, Ebola in 2014–16 and Zika in 2015–16.
What stopped these outbreaks wreaking global havoc was usually one or more of these factors: poor infectivity (MERS), a relatively low fatality rate (swine flu) or a swift, co-ordinated international response (SARS). In other words, good luck and good preparation working in tandem.
In a sense, we got lucky with Covid-19, despite the fact that it caused 20 million or more deaths across the world. The point is that the vast majority of people infected with the virus managed to recover.
Ebola, on the other hand, has a fatality rate of around 67 per cent. Bird flu is not far behind at 60 per cent. Even MERS hit 34 per cent.
So we certainly can’t bank on the next pandemic being easily contained.
Imagine Disease X is as infectious as measles with the fatality rate of Ebola. Somewhere in the world, it’s replicating, and sooner or later, somebody will start feeling sick.
So why are pandemics on the increase? Well, I can assure you that we’re not simply experiencing a random patch of bad luck.
The increase in outbreaks is the price we’re having to pay for living in the modern world. First, it’s increasingly connected through globalisation. Second, more and more people are cramming into cities, where they often come into close contact with others.
And third, millions of acres of natural habitat are being destroyed by us each year. This reason is particularly important, because around three-quarters of emerging infectious diseases originate in animals and then leap from species to species until they can, in certain circumstances, infect human beings.
Through deforestation, modern agricultural methods and the destruction of wetlands, we are creating the ideal conditions for these species jumps to take place.
Why? Because massive loss of habitat is pushing animals into ever closer proximity to different species — including us. It’s a virus’s idea of paradise.So what’s to be done? Crucially, we need to take the first steps in dealing with the next pandemic right now — and that involves putting money on the table.
Pandemic viruses have a lot in common with software viruses, which most of us take very seriously. So we invest in the appropriate software, and we update it regularly on our phones, tablets, laptops and desktops.
We don’t just sit back and hope we’ll never be victims of a computer virus attack. On the contrary, most of us spend quite a bit to ensure we won’t.
In 2020, the cybersecurity market globally was valued at a little under $170 billion; at current growth rates it will hit almost $370 billion by 2028. That’s an astonishing amount of money.
Yet there’s very little evidence that we’re prepared to spend anything remotely comparable on protecting ourselves from real viruses — the ones that could kill us.
Yet the monetary cost of inaction is seismic. After all, even Covid-19 — a milder virus than Disease X — managed to leave us holding a bill for $16 trillion in both lost output and public health expenditure.
That’s why we need to discover — in advance of the next pandemic — a collection of different prototype vaccines for every threatening virus family that we know about. We’d then have a head start — because we’d be able to engineer those vaccines to target the very specific features of Disease X.
Impossible? Not at all.
The reason why there was such a rapid global response to Covid-19 was because frameworks had already been developed a decade earlier as part of the (unsuccessful) process to develop vaccines against SARS and MERS.
So when Covid-19 emerged, scientists already had a prototype design that could be modified to deal with the new virus.
Developing appropriate vaccines in less than a year was something of a miracle. Yet even that speed would be insufficient if the next pandemic turns out to be far more lethal than the last.
When I led the Vaccine Taskforce, a central feature of our approach was to build a portfolio of different types of vaccines. In 2020, we didn’t know which, if any, format of vaccine was going to work against Covid-19 and its variants, so we wanted to deploy a breadth of different approaches.
To deal with Disease X, we’ll again need a portfolio strategy.
First, because different types of vaccines stimulate different immune responses and therefore they provide different levels of protection.
Second, manufacturing capabilities vary enormously across countries and regions.
Some vaccine formats may be suitable for large-scale production, while others may be easier to produce in the third world.
We saw this with Covid-19, where it made sense to use Pfizer-BioNTech and Moderna in wealthier nations and Oxford-AstraZeneca in poorer places.
Third, we need to address the shortcomings of current vaccines, not all of which are durable, easy to transport or cheap.
Fourth, researchers must be encouraged to trial new technologies and approaches to vaccine design, potentially leading to more effective and efficient vaccines in the future.
Vaccines aren’t the only answer, of course. We urgently need to invest in state-of-the-art systems for international surveillance of prospective virus threats.
Ideally, Disease X will be neutralised before it starts spreading across the globe and mutating (which it certainly will, if left unchecked).
We also need to think again about what can be done during the period after Disease X hits Britain, and before an effective vaccine can be rolled out.
In 2020, we had no experience of lockdowns, so it was painfully obvious that policy was made up on the hoof. No such excuse next time.
Before it even enters Britain, we need to have rehearsed our response much better and more scientifically. Was it right to close schools? To lock down for long periods? To ban travel? Advise people to wear masks?
Researchers are working on these questions, among others. But there should be no restrictions on who can work on the data from the last pandemic — it should be made available in a central database to scientists around the world.
We need to go even further. One of the many tragedies of the 2020 Covid-19 saga was that countries often retreated into silos and failed to support any serious international plan. It was a major failure, which cost many lives.
To provide vaccines at low cost, we must build biological vaccine-manufacturing capacities in countries from each continent, and organise robust training. Ideally, the countries selected would be ones with low populations.
Why? Because there would be less chance of political demands to ‘vaccinate our own people first’ rather than treating those most in need. The vaccine nationalism of 2020, one hopes, would become a thing of the past.
This really is no time for complacency. We’ve already experienced a relatively non-lethal pandemic, and governments are aware that the next one could be far worse.
The logical next step is to have a single global body responsible for our response to Disease X. The obvious one to take up the mantle is the Coalition for Epidemic Preparedness Innovations (CEPI), working in close conjunction with the World Health Organisation.
Truly international, CEPI was launched at Davos in 2017 to develop vaccines against future epidemics. It is currently working on a five-year plan to compress vaccine development to 100 days and create a library of vaccines.
We will also need to fund a global budget for this body, with contributions based on national wealth.
Finally, all of them should agree to sign up to a Global Pandemic Treaty. This would enable the open sharing of information among scientists and clinicians, and give clear accountability for vaccine development and manufacturing.
A tall order? Perhaps — but not an impossible one.
The remarkable success of the scientific drive against Covid-19 shows what can be achieved when we pull together. But next time, we need to be far better and far faster.